In this blog post I will look at what an abreaction is. I will explore how it fits into our work as therapists and how we can work with that abreaction. If that sounds like it may be interesting to you, please do read on.
What is an abreaction?
Abreaction is a term that has it’s origination in Psychoanalysis. The Collins dictionary defines in as “the release and expression of emotional tension associated with repressed ideas by bringing those ideas into consciousness.”
There can often feel like there’s a lot of judgement about abreactions. Almost that they shouldn’t happen and they are a bad thing. I can certainly remember my early days in using EMDR. Sometimes the intensity of the emotion expressed by the client would cause strong emotion in me as a therapist. Was this ok? Could I contain it? Was the client benefiting? Had I caused the client to get emotional? Am I retraumatising the client? Am I a terrible therapist?
When I reflect back, I believe that EMDR is a bit like that Heineken advert. It hits the spots other therapies don’t reach. So I found that my EMDR sessions got very emotional, very quickly. I simply had not noticed it happening that fast in the other therapy models. My experience was based on CBT or Psychodynamic Psychotherapy.
So the window of tolerance has helped me to feel more contained when thinking about an abreaction
The window of tolerance.
The window of tolerance is like a sash window. A window that can increase or decrease at any one time. The depth of it often changes during a therapy session. We as therapists have to consider whether our clients are in their window of tolerance. Our clients need to feel grounded, safe but in touch with their emotions. We are judging the level of intense emotion the client is experiencing we don’t want it too high that the client become hyperaroused or too low that they are numb and detached. It takes a lot of skill and therapeutic alliance to recognise where a client might be.
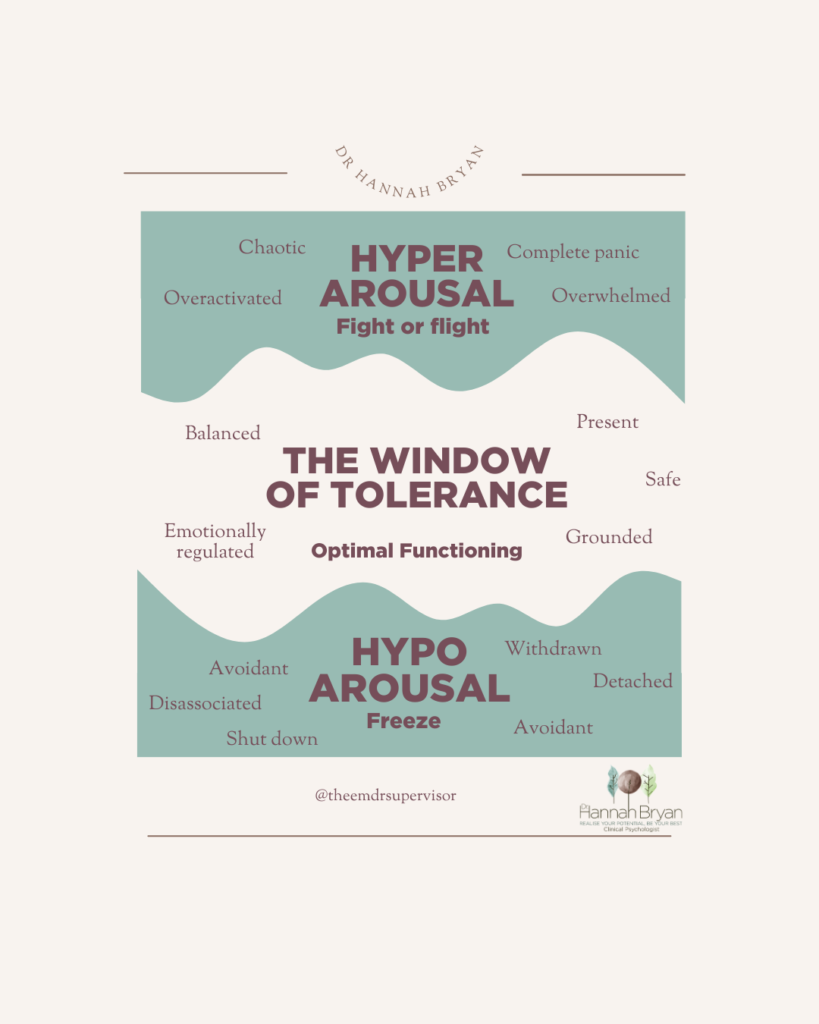
Does the emotion come and the client switches off? They might go to a numb space and below the window of tolerance. They might feel nothing and just be detached from the emotion. Maybe this is the client being below their window of tolerance.
Or does the emotion appear and it becomes too much, it’s unbearable. The clients thinking brain has gone off line. It’s all just too much. The client is possibly above their window of tolerance.
Abreactions are often helpful to our clients working through their traumas
I have learnt to sit with a client and their emotion. To get a sense for whether this is emotion and an abreaction that just needs to be worked through. Or actually is the client going out of the window of tolerance and needs grounding a little before continuing. I believe this takes work to grow this understanding with our clients.
In my experience, most of the time, if it’s early days of working through a trauma memory, I am now actually expecting and hoping for an abreaction. If we think of it within the AIP model (Adaptive information processing) all we are trying to do is process and work through the feelings, experiences, memories that are attached to a trauma memory. This is a process of releasing so we have to get in touch with that emotion to be able to deal with it.
Helping clients to build their confidence in the process.
We always teach clients the stop signal in EMDR 🤚. The client is navigating their journey. We use phase 2 preparation to make sure our client has enough skills in their toolbox to help them tolerate difficult emotions. As Glennon Doyle says in her book Untamed, “We can do hard things” and let’s never forget that. We will also in preparation talk a little about the process of EMDR. We will say it may or it may not be emotional but the clients job is just to let what happens happen.
You’ve got to feel to heal
I regularly find myself emphasising how important it is now to feel to heal. For me part of the recovery journey is allowing ourselves to be in touch with all the emotion we feel about a particular situation. However I certainly remember a time when I didn’t think this way. When I was almost fearful of the emotion that might be expressed in the clinic space and sometimes even trying to prevent it from being there. I’m cringing a little as I write this bit. But it’s so true as our clients grow through the experience of therapy, so do we as therapists. I’m grateful to all my clients for allowing me to share in that joint growth journey.
Working in the session with abreactions
When there is an abreaction in sessions, I generally am more active rather than the default position of staying out of the way. I might say “It’s old distress” “You’re safe now” “you’re doing really well” a little more often that usual. Use of these light, gentle words helps to keep the client grounded. It lets them know that I am here, on the journey with them.
I pay extra attention to the client , I notice their breathing rate, body tension and the tears. I will tend to let the Bilateral Stimulation run for longer. When I see a pause than I will pause the BLS. This might be something like the client taking a deeper breath. They might drop their shoulders a little. We might see a change in their facial expressions. As a therapist we are constantly paying close attention to what is happening in the room. Whether that’s the zoom room or the therapy room.
I see the emotion as being a hill that we have to go up and then come down the other side. When I think the clients have come over the peak of the emotion that’s when I will pause the BLS. I will often try and activate the parasympathietic system a little more. I might ask the client to take a deep breath and then it’s the usual “What do you get know” then “go with that”.
What happens after an Abreaction
The client usually comes out the other side. Often, and especially in the early days, I have had to learn to sit with my fears. I would front load my own AIP system and remind myself the whole theory of EMDR, that current difficulties are connected back to unprocessed traumatic experiences. It then makes obvious sense that we need to work through the emotions that are connected to these experiences and that is my default emotional work.
Boy it’s tough being an EMDR therapist! If you are working towards EMDR Accreditation, have a look at my Demystifying the EMDR Accreditation process workbook Click here.
Did you know I run a webinar series to support therapist in building their knowledge and skill in EMDR? Click here to find out more.
Who am I?

Hi, my name is Dr Hannah Bryan and I am a Chartered Clinical Psychologist and a Europe Approved EMDR Consultant and Facilitator. In 2006 I trained as an EMDR therapist. I have been an EMDR Consultant since 2014 and an EMDR Facilitator since 2019.
I am extremely passionate about helping clinicians improve their knowledge and skills in EMDR so that they improve their confidence and practice it more with their clients and more clients recover and heal from the traumas they have experienced.

0 Comments